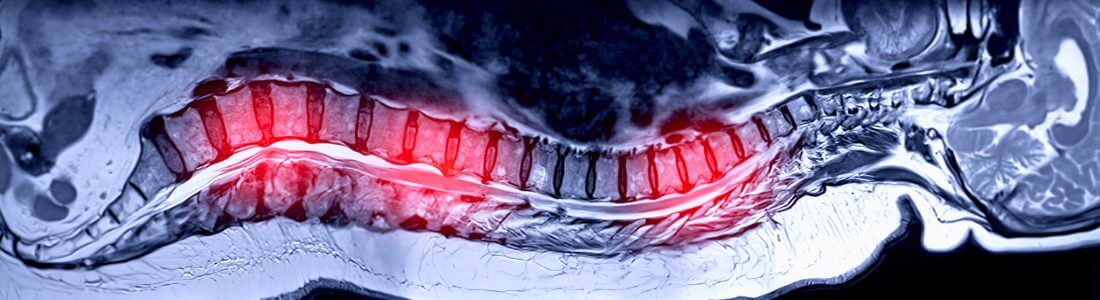
A pain pump is a medical device which delivers medication directly into the intrathecal space around the spinal cord. Consequently, it is more properly referred to as an intrathecal drug pump. The device is surgically implanted, usually into the abdomen, with the medication delivered into the intrathecal space through a small catheter.
To be clear, the fitting of a pain pump is a major procedure usually only contemplated if pain relief cannot be achieved by less invasive means. That is why it is common to find it used in palliative care for the delivery of morphine. Infections, internal bleeding and fluid leaks are just a few of the possible complications. Added to that, the device’s medication reservoir must be topped up regularly via a needle through the skin.
Advantages
A pain pump administers medication directly into the cerebral spinal fluid that surrounds the spine. As the medication is delivered so close to the spinal cord, a lower dose is usually required (but see below) resulting in less side effects from the medication. An added advantage is that it takes effect faster than medication taken orally.
Disadvantages
The main disadvantages are outlined above – the surgical and related risks and the need to regularly top up the device’s medication reservoir (usually every one to three months).
Pain pumps are only rarely considered for people suffering CRPS. There is no research supporting their long term benefit for the condition. In fact, it has been found that where fitted to people with CRPS, their tolerance to the medication can increase over time, in turn increasing the amount of medication required for pain relief. Eventually, the pain pump may become virtually ineffective and further surgery to remove it may then be considered.
In one small scale study the results of which were published in 2009, 42 CRPS patients received baclofen via intrathecal pump to ascertain its benefit on CRPS-related dystonia. Of those, 38 were then followed up for 12 months. In conclusion, the researchers reported:
“Dystonia, pain, disability and [quality of life] all improved on intrathecal baclofen (ITB) and remained efficacious over a period of one year. However, ITB is associated with a high complication rate in this patient group, and methods to improve patient selection and catheter-pump integrity are warranted.”
Whilst the results of that trial were generally positive, the high risk of complications tends to relegate pain pumps to a lowly position in the list of treatment options for CRPS.
Pain pumps are not the only subcutaneous device fitted for the relief of pain. In a number of earlier articles on this Blog we have discussed spinal cord stimulation (SCS) for CRPS. Whilst there is no definitive protocol on the subject, it seems that often where pain pumps are implanted, SCS has already been tried unsuccessfully.
You may also be interested in the following articles:
Hushed up? Could a simple antibiotic successfully treat therapy-resistant CRPS?
Can Plasma Exchange Therapy help severe, longstanding CRPS?