In recent years, spinal cord stimulation (SCS) has become an increasingly common tool in the management of long-term neuropathic and other pain conditions. Indeed, earlier this year the National Institute for Health and Care Excellence (NICE) recommended that along with more general multidisciplinary input, people with chronic post-operative neuropathic back or leg pain should have access to newer high-frequency SCS.
New science
It is over 50 years since the first, rudimentary ‘stim’ was implanted. Despite the passage of time and the development of increasingly sophisticated devices, SCS remains relatively new science, with little true understanding of either its mechanism or the effect on the body of short, medium and long term electrical stimulation.
Gate control theory of pain
In the late 1960s, SCS was a direct response to the then-new gate control theory of pain. The following short clip is a beautifully over-simplified explanation of the theory, but one that even I can follow!
Among other things, the gate control theory predicted that the electrical stimulation of nerve fibres would alleviate both chronic neuropathic and acute nociceptive pain. However, while SCS can alleviate neuropathic pain, it has little effect on nociceptive pain, suggesting that SCS does not act simply through the electrical stimulation of nerve fibres and that some other mechanism is also involved.
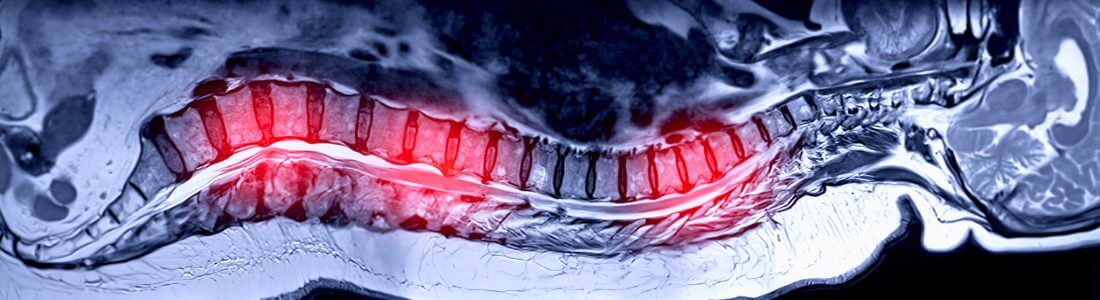
Indeed, while electrical stimulation can lead to pain reduction, which can be visualised through medical imaging as changes in brain activity, research has revealed that it can also lead to neurochemical and physiological changes in the spinal cord.
Swedish study
A study at the University of Uppsala in Sweden investigated the effect of SCS on proteins in the cerebrospinal fluid (CFS) which surrounds the brain and spinal cord. They discovered that:
“Eighty-six proteins were statistically significantly altered in the CSF of neuropathic pain patients using SCS, when comparing the stimulator off condition to the stimulator on condition.”
What does this tell us?
At first glance, the discovery of these chemical changes may not appear to tell us a great deal. However, the researchers acknowledge that knowing the identity of the proteins affected, and in which body process each is involved, is helping to “expand the picture of SCS effects on the neurochemical environment of the human spinal cord.”
In turn, “An improved understanding of the SCS mechanism may lead to new tracks of investigation and improved treatment strategies for neuropathic pain.”
Watch this space.
You may also be interested in the following articles:
Spinal Cord Stimulation during pregnancy
Are Dorsal Root Ganglion (DRG) Stimulators set to replace Spinal Cord Stimulators (SCS)?
Spinal Cord Stimulation: Low Frequency vs High Frequency